Inflammatory Breast Cancer in Canada: An Overview
How do I know if I have IBC?
Breast health starts with knowing your breasts so that you are more likely to notice changes that may lead you to get them checked out. Know your body. Know IBC.
Inflammatory Breast Cancer is a rare and aggressive form of breast cancer, believed to account for approximately 1-5% of all breast cancer diagnoses in Canada based on data from other countries like the US and the UK. While specific Canadian statistics are limited, the challenges posed by IBC remain significant due to its aggressive nature and the urgency required for its timely diagnosis and treatment. In most cases, inflammatory breast cancer has already spread to the lymph nodes or other organs when it is diagnosed.
Inflammatory Breast Cancer is characterized by cancer cells blocking lymph vessels in the skin of the breast. This blockage leads to the breast often looking swollen, red, or “inflamed”. These symptoms can easily be mistaken for an infection like mastitis.
RISK FACTORS
Inflammatory breast cancer shares many risk factors with other types of breast cancer. These include:
AGE
Breast cancer risk generally increases with age. IBC is typically diagnosed around age 51, which is slightly younger than other types of breast cancer.
Obesity
Being overweight, especially after menopause, raises the risk of breast cancer.
Dense breast tissue
Dense breast tissue, visible on mammograms, is associated with an increased risk of breast cancer.
Genetic mutations
Specific mutations in genes like BRCA1 and BRCA2, can increase the risk of breast cancer. Other mutations in genes like PALB2, CHEK2, and PTEN are also linked to breast cancer risk. While no mutations are specifically associated with IBC, research continues to explore the role of genetics in this form of cancer.
Family History
Having a first-degree relative (parent, sibling, or child) with breast cancer increases the likelihood of developing the disease.
Early menstruation
Starting menstruation before age 12 raises the risk of breast cancer.
Pregnancy history
Women who haven’t had a full-term pregnancy or who had their first full-term pregnancy after age 30 have a higher breast cancer risk.
Previous breast cancer
Having had breast cancer previously increases the risk of developing it again.
Previous radiation therapy
Radiation treatment to the chest in childhood or early adulthood, while beneficial for treating other conditions, can increase the risk of breast cancer later in life.
These factors collectively contribute to the risk profile for developing inflammatory breast cancer.
Symptoms of Inflammatory Breast Cancer
Unlike other breast cancers, Inflammatory Breast Cancer symptoms are noticeable soon after it develops. It is important to note that many women with IBC do not find a lump.
Common Symptoms of IBC
IBC symptoms can appear suddenly, often within days or weeks, making early detection crucial. IBC symptoms vary between individuals and may include:
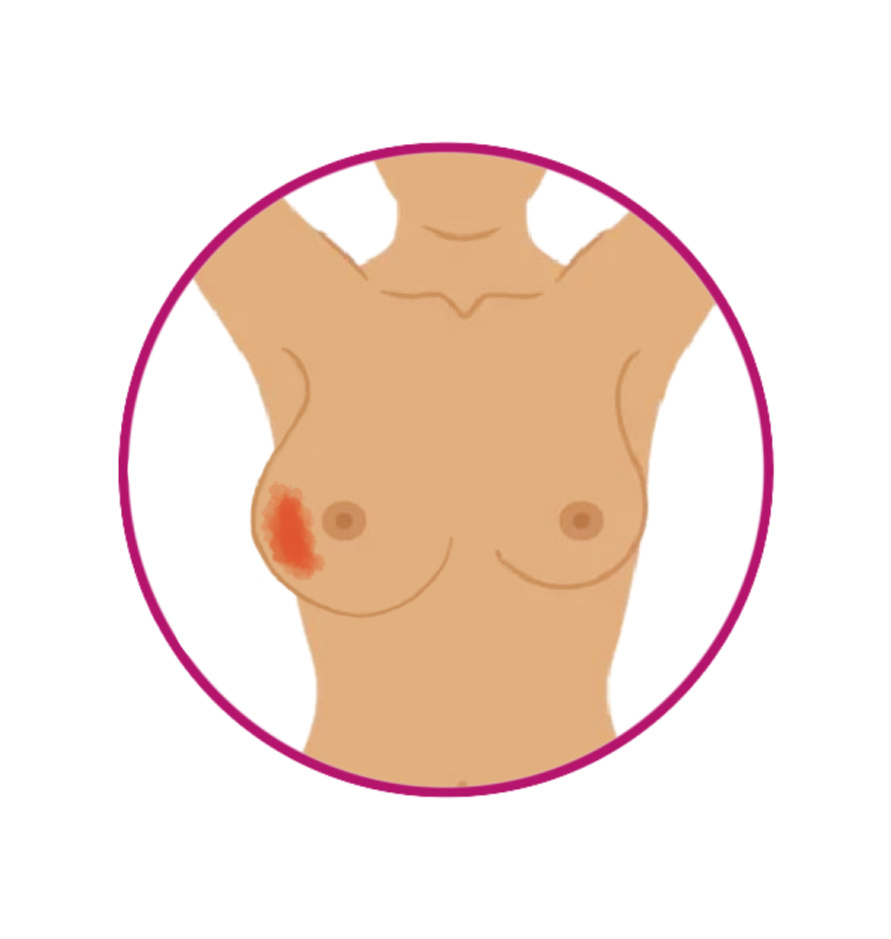
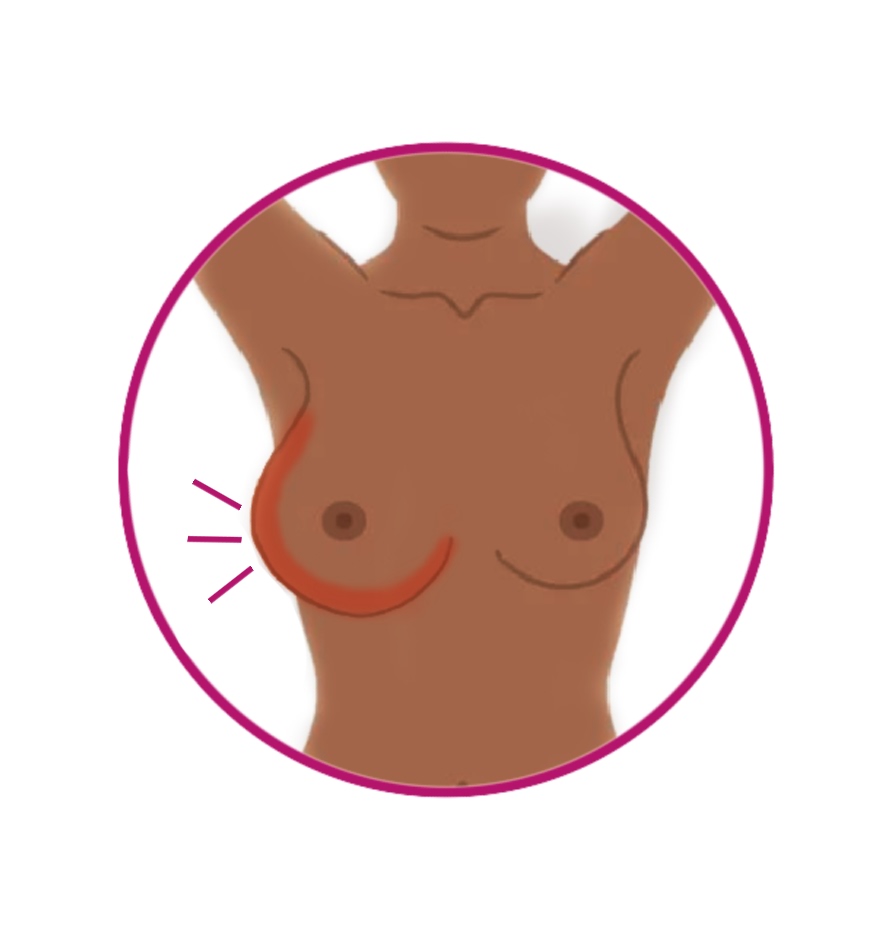
Skin Discoloration
One of the most common symptoms is a change in the skin’s colour, with the skin on at least one-third of the breast becoming red, pink, purplish or darkened.
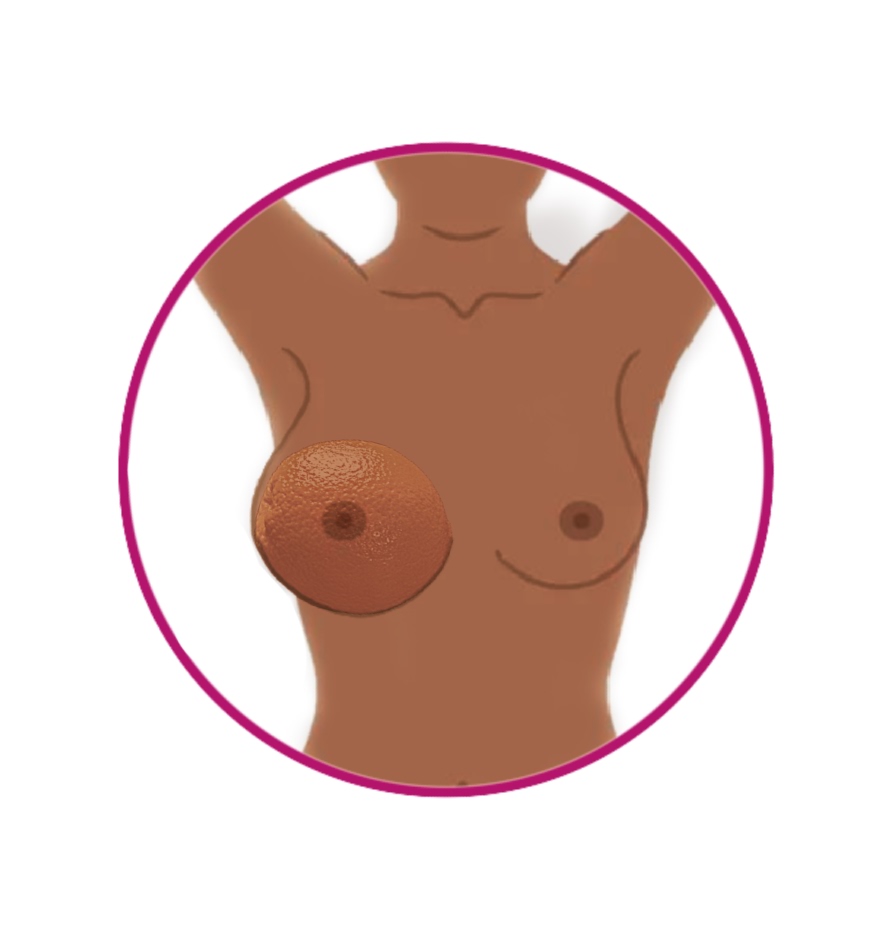
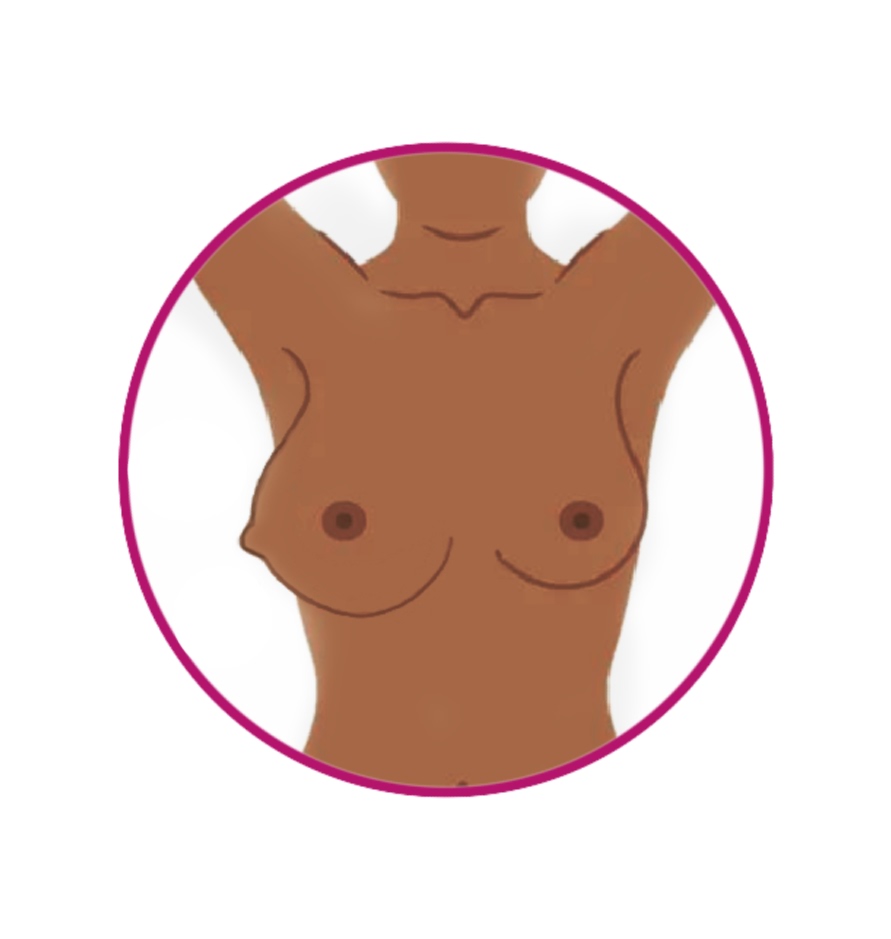
Orange Peel Skin
The skin might also appear dimpled or pitted, resembling the texture of an orange peel, a condition known as peau d’orange.
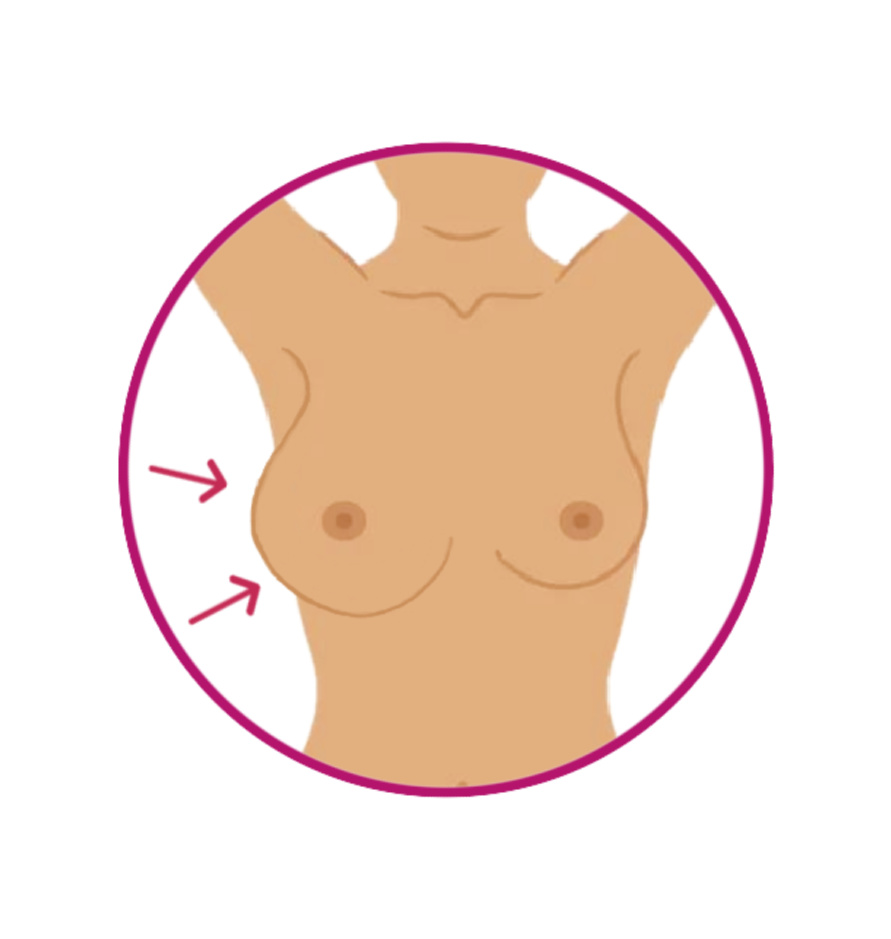
Breast Swelling
Sudden swelling of the breast, often with one breast becoming much larger than the other.
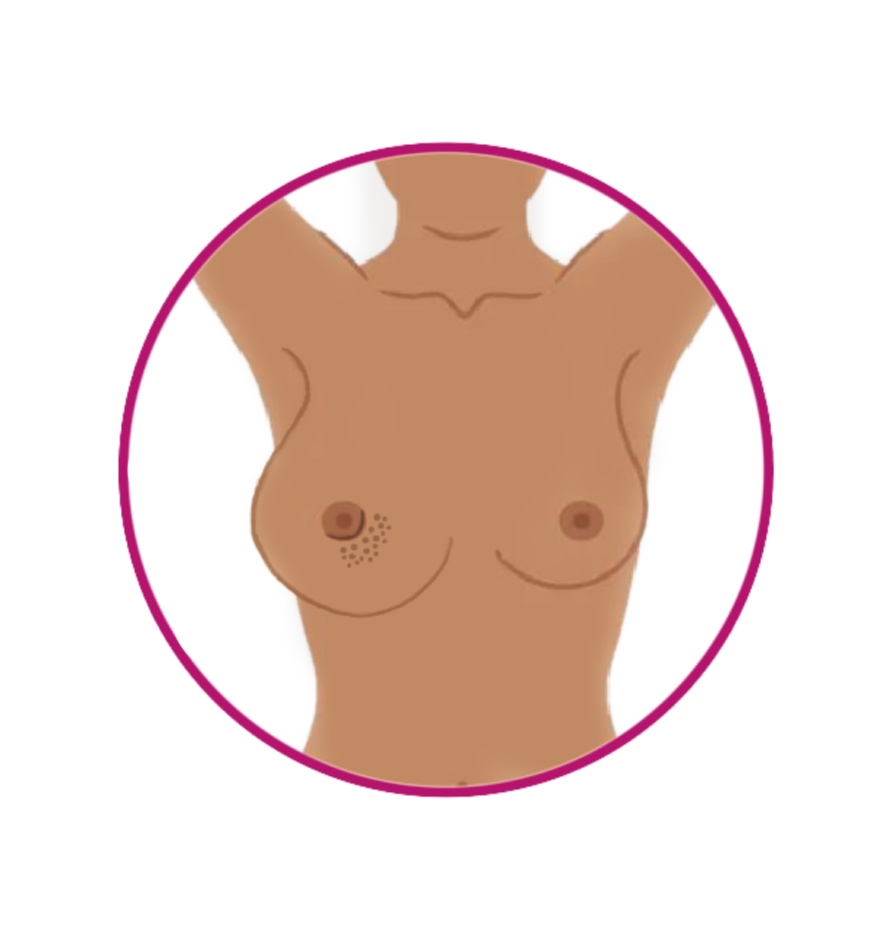
Thickened Skin or Tissue
The skin or tissue of the breast may feel thicker than usual, or there might be noticeable ridges.
Warmth
The affected breast might feel warm to the touch.
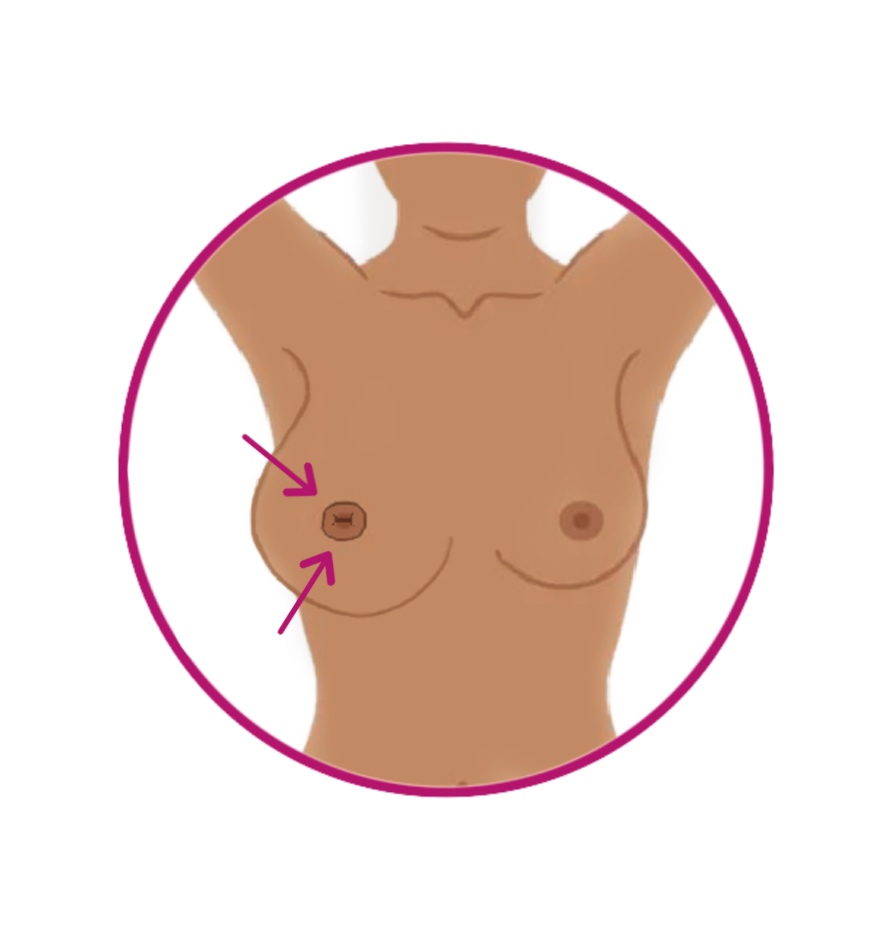
Nipple Changes
The nipple may flatten, retract, or suddenly point inward (a condition known as an inverted nipple).
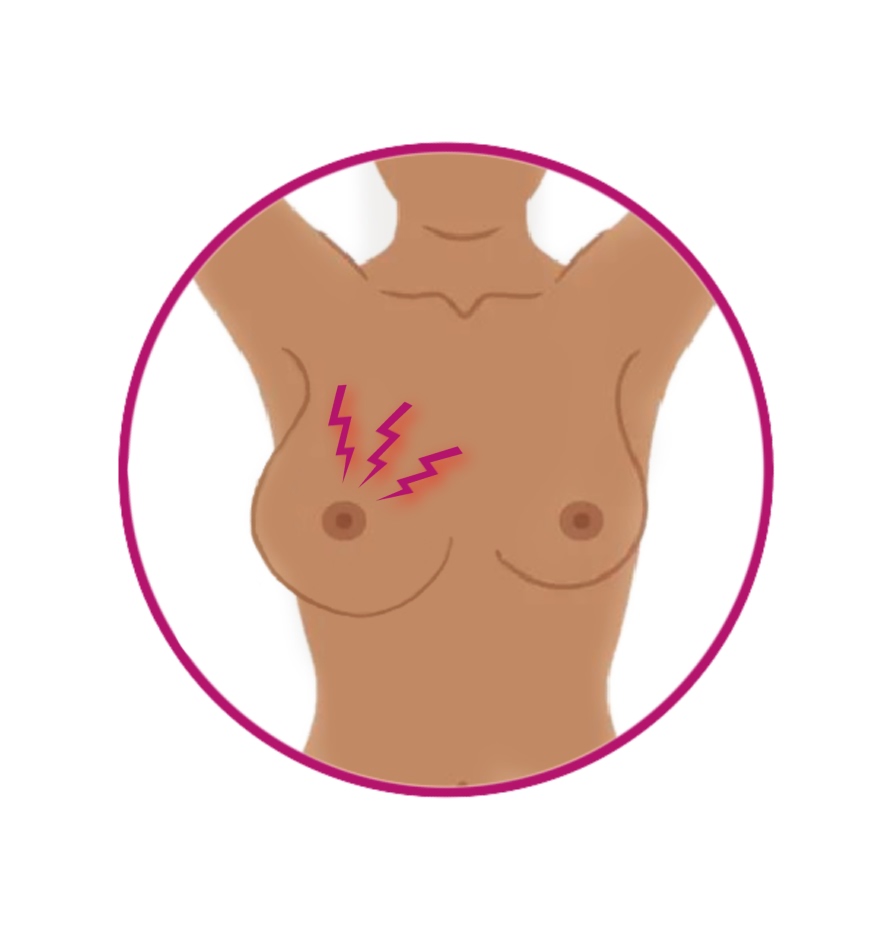
Tenderness and Pain
The breast might be tender and some may experience itching, burning or shooting pain.

A "bug bite" or Swollen Lymph Nodes
- A “bug bite”: or a small pimple or blister like lesion that doesn’t heal
- Swollen Lymph Nodes: The lymph nodes near the armpit (axilla) or near the collarbone may be swollen.
Lump
While most women with IBC do not find a lump in the breast, it is possible.
Important Considerations
To be classified as inflammatory breast cancer, though, the skin changes must:
- have occurred within the last 6 months, and
- involve at least a third of the breast.
The symptoms of IBC can be easily mistaken for an infection in the breast tissue, known as mastitis, which is more common in breastfeeding women. However, IBC symptoms do not respond to antibiotics. If you experience any of these symptoms, it’s vital to consult your doctor immediately, as waiting for antibiotics to work may delay the diagnosis and treatment of IBC.
IBC is typically diagnosed at an advanced stage, usually Stage 3 or Stage 4, meaning it has spread into surrounding tissues or beyond. While IBC is usually associated with locally advanced breast cancer, it is distinct in its rapid progression and early spread. Early recognition and prompt action are crucial for managing this aggressive cancer.
Breast Self-Exams for Early Detection of IBC Symptoms
Regular breast self-exams are crucial for early detection, especially for those at risk of Inflammatory Breast Cancer. Here’s how to perform them effectively.
Performing a Breast Self-Exam:
- Step 1: Stand in front of a mirror with your shoulders straight and arms on your hips. Check for any changes in size, shape, or color, and note any visible distortion or swelling.
- Step 2: Raise your arms and look for the same changes.
- Step 3: While lying down, use your right hand to feel your left breast and your left hand to feel your right breast. Use a firm, smooth touch with the first few fingers of your hand, keeping the fingers flat and together.
- Step 4: Cover the entire breast area, from your collarbone to the top of your abdomen and from your armpit to your cleavage.
- Watch for IBC-Specific Symptoms: Be aware of redness, swelling, warmth in the breast, skin changes (like thickening or an orange-peel texture), or unusual nipple discharge.
- Visual Aids: Use diagrams or watch this video tutorial on breast self-exams for additional guidance.
Call to Action: Perform regular self-exams and consult your doctor immediately if you notice any unusual changes.
Diagnosing Inflammatory Breast Cancer
Understanding an IBC Diagnosis
Diagnosing Inflammatory Breast Cancer can be challenging due to its rapid progression and similarity to other conditions. Here’s what you need to know about diagnosing IBC:
Diagnostic Criteria
- AJCC Staging: IBC is classified as T4d in the American Joint Committee on Cancer (AJCC) Tumor, Node, Metastasis (TNM) staging system. This designation reflects the advanced nature of the disease, indicating significant involvement of the breast tissue and surrounding areas.
IBC Scoring System
What Is the IBC Scoring System?
The Inflammatory Breast Cancer Scoring System is a specialized tool designed to help healthcare providers accurately identify IBC cases. It aims to improve the diagnostic process, guide treatment decisions, and support research efforts.
This system was created through a collaboration between Susan G. Komen, the Inflammatory Breast Cancer Research Foundation, and the Milburn Foundation. Experts—including doctors, researchers, and IBC patients—worked together to establish clear diagnostic criteria based on the key clinical, pathological, and imaging characteristics of IBC.
The scoring system is currently being validated by researchers at two of the world’s largest IBC centers, led by Dr. Filipa Lynce at Dana-Farber Cancer Institute and Dr. Wendy A. Woodward at MD Anderson Cancer Center.
How Does It Work?
Healthcare providers use the IBC Scoring System by entering detailed information about a patient’s symptoms, imaging results, and pathology findings. The system then calculates a score that falls into one of four categories:
- Very Likely IBC: Symptoms and findings strongly indicate IBC.
- Strong Possibility of IBC: A high likelihood that the symptoms could be IBC.
- Weak Possibility of IBC: IBC is possible, but less likely based on the symptoms.
- Very Unlikely IBC: IBC is unlikely, though other breast conditions may be considered.
Important Considerations
- Not a Standalone Diagnosis: The IBC Scoring System is not a diagnostic tool by itself. A confirmed diagnosis of IBC requires a biopsy to detect the presence of breast cancer cells. This tool is particularly helpful in differentiating IBC from other types of breast conditions.
- Subjectivity and Ongoing Validation: The system is still undergoing validation, meaning it’s being tested and refined to ensure its accuracy and reliability. Some aspects of the scoring may be subjective, and healthcare providers are encouraged to provide feedback to improve the tool.
- Advocacy Tool for Canadian Patients: While this system is not specific to Canada, it can still help patients advocate for a timely diagnosis by providing structured information to discuss with their healthcare team.
- Work with Your Healthcare Provider: If you’re concerned about IBC, discuss your symptoms with your doctor. They can use this system as part of a broader diagnostic process to determine the best next steps.
For more detailed information on how the scoring system was developed and its scientific basis, refer to the publication: “Inflammatory breast cancer defined: proposed common diagnostic criteria to guide treatment and research” (Breast Cancer Res Treat 2022 Apr;192(2):235-243).
Primary vs. Secondary IBC
- Primary IBC: Refers to cancer that originates in a previously normal breast. This is when the disease develops without any prior history of breast cancer.
- Secondary IBC: Occurs when inflammatory changes develop in a breast already affected by invasive cancer of following surgery for a non-inflammatory form of breast cancer.
Symptom Overlap with Mastitis
- IBC symptoms can closely resemble those of mastitis, an infection more common in breastfeeding women. Symptoms such as redness, swelling, and warmth in the breast may lead to confusion between the two conditions.
- Doctors might initially treat suspected mastitis with antibiotics. However, if these treatments do not resolve the symptoms, it may delay the correct diagnosis of IBC. Timely diagnosis is crucial because IBC progresses rapidly and can significantly impact treatment outcomes.
Recognizing the Rapid Progression
- IBC is diagnosed at later stages (Stage III or IV) due to its aggressive nature and the difficulty in identifying its symptoms early on. The disease can escalate from a small change in skin appearance to a fully involved breast within weeks, and in some cases, even overnight.
- Typically classified as locally advanced breast cancer, IBC means that the cancer has spread into nearby tissues but may not have yet reached distant parts of the body. Early and accurate diagnosis is essential for effective treatment.
Importance of Early Detection
- Awareness and prompt evaluation of any changes in breast appearance are critical. If you notice any unusual symptoms or changes in your breast, seek medical advice without delay. Early detection can greatly improve treatment options and outcomes.
Diagnostic Tests
To diagnose IBC and determine its stage, various tests may be used:
- Clinical Breast Exam: An initial physical examination to assess any abnormalities in the breast.
- Diagnostic Mammogram: An X-ray of the breast to look for any unusual changes.
- Breast Ultrasound: Uses sound waves to create images of the breast tissue.
- MRI of the Breast: Provides detailed images to assess the extent of the cancer.
- Digital Mammogram: A more advanced form of mammography that can offer clearer images.
- Core Biopsy of the Breast: A procedure to remove small samples of breast tissue for analysis.
- Skin Punch Biopsy: A technique to take a sample of the skin for examination, especially important for diagnosing skin changes in IBC.
- Hormone Receptor Status Testing: Determines if the cancer cells have hormone receptors, which can influence treatment options.
- HER2 Status Testing: Identifies if the cancer cells overexpress the HER2 protein, which can guide targeted therapy decisions.
-
Molecular Subtypes of IBC
Inflammatory Breast Cancer, like other forms of breast cancer, can be classified into four molecular subtypes based on hormone receptor status, HER2 expression, and proliferation rate (how quickly cancer cells are dividing and growing), based on the AJCC molecular classification, as summarized in the American Journal of Roentgenology (AJR, 2020):
- Luminal A: High estrogen (ER) and progesterone (PR) receptor expression, low proliferation rate, and usually HER2-negative. This subtype generally has the most favorable prognosis.
- Luminal B: Lower ER/PR expression with a higher proliferation rate, meaning it grows more aggressively. It is usually HER2-negative, but about 30% of cases are HER2-positive.
- HER2-enriched: HER2-positive with either positive or negative hormone receptor status. These cancers are typically high-grade with a high proliferation rate, but HER2-targeted therapies, such as trastuzumab, have significantly improved outcomes. (HER2-positive means the cancer has too much HER2 protein, while HER2-enriched is a specific molecular subtype that tends to grow faster. Not all HER2-positive cancers are HER2-enriched.)
- Basal-like (often Triple-Negative): Lacks ER, PR, and HER2 expression and has a high proliferation rate, making it one of the most aggressive subtypes with fewer targeted treatment options.
Compared to other types of breast cancer, IBC is more frequently associated with the HER2-enriched or basal-like (triple-negative) subtypes, which influences both treatment options and prognosis.
Challenges in Diagnosis
- Symptom Overlap: IBC symptoms can closely resemble those of mastitis, an infection more common in breastfeeding women. Symptoms such as redness, swelling, and warmth in the breast can lead to misdiagnosis. Many cases are initially treated as mastitis with antibiotics, which may delay the correct diagnosis if symptoms persist.
- Screening Limitations: IBC is not easily detected by standard mammograms and often does not present with a palpable lump, making it harder to identify through routine screenings. This can result in prolonged diagnostic journeys, especially in cases where healthcare providers may lack specific training or experience with IBC.
- Need for Awareness: There is a critical need for improved education and training about IBC among healthcare providers, including midwives, nurse practitioners, and general practitioners to expedite the timeline from diagnosis to treatment. Increased awareness can help in the early and accurate diagnosis of this rapidly progressing cancer.
